Levelling the Playing Field: Resource Stratification, Decentralised Trials and Accessible Therapies
As part of World Cancer Day (4th Feb), the journal of Molecular Oncology invited researchers to take part in a writing competition aimed at highlight existing or future policies directed at making cancer treatment equally accessible to all patients both locally and globally. This entry, by Shan Sunny (University of Leeds School of Medicine, UK), received the second prize.
Despite remarkable advances in oncology, inequitable cancer care prevails. High-income countries capitalise on their advanced diagnostics, precision medicine, and well-established treatment infrastructure. Conversely, low and middle-income countries (LMICs) persistently face the silent epidemic of late-stage cancer diagnoses and suboptimal treatment, that is limited by resource deprivation (Oluwaseun Adebayo Bamodu and Chung, 2024). According to the World Health Organization, approximately 70% of global cancer deaths occur in LMICs, underscoring the need for systemic change (WHO, 2018). Such reforms are achieved through evidence-based, scalable strategies and policy solutions like global resource stratification frameworks (National Comprehensive Cancer Network, 2025), decentralisation of clinical trial networks, and drug pricing reform through compulsory licensing (De las Heras et al., 2022).
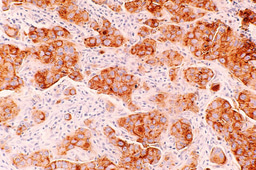
A universal, "one-size-fits-all" approach to cancer treatment is neither tenable nor effective. The Breast Health Global Initiative created a resource stratification framework classifying interventions based on the available infrastructure into four levels: basic, limited, enhanced and maximal (Duggan et al., 2020). To enhance resource allocation and equity, this framework should be applied to all cancers. Malawi, a compelling example, has set its cancer screening policy according to resource availability, wherein Visual Inspection with Acetic Acid remains the predominant screening method due to its ease of use and low cost (Msyamboza et al., 2016). The minimal infrastructural needs have enabled trained health workers to successfully undertake cancer screening in environments where resources are constrained (Kamaraju et al., 2020). Consequently, integrating specific resource-oriented interventions alongside adapting cancer-care models to different levels of healthcare infrastructure, may address the absence of radiotherapy, chemotherapy, and surgical treatment options in low-resource settings (Hunter et al., 2020).
Although clinical trials underpin oncological progress, over 80% are conducted in Europe and North America, restricting diversity and denying LMICs early therapeutic access (Drain et al., 2018). Therefore, scaling decentralised clinical trials could revolutionise global oncology research. As demonstrated during COVID-19, telemedicine, mobile study units, and electronic portals could be used to extend the reach of trials (Adams, Long and Fleury, 2022). For example, the PROSE study in Nigeria utilised remote trial strategies to improve participation and symptom monitoring during cancer treatment (Salako et al., 2023). If regulatory bodies like the FDA and EMA mandated 10-15% of trial sites to be in LMICs or encouraged greater remote involvement, an immediate improvement in drug access equity and research generalisability may be observed (Ndembi et al., 2024).
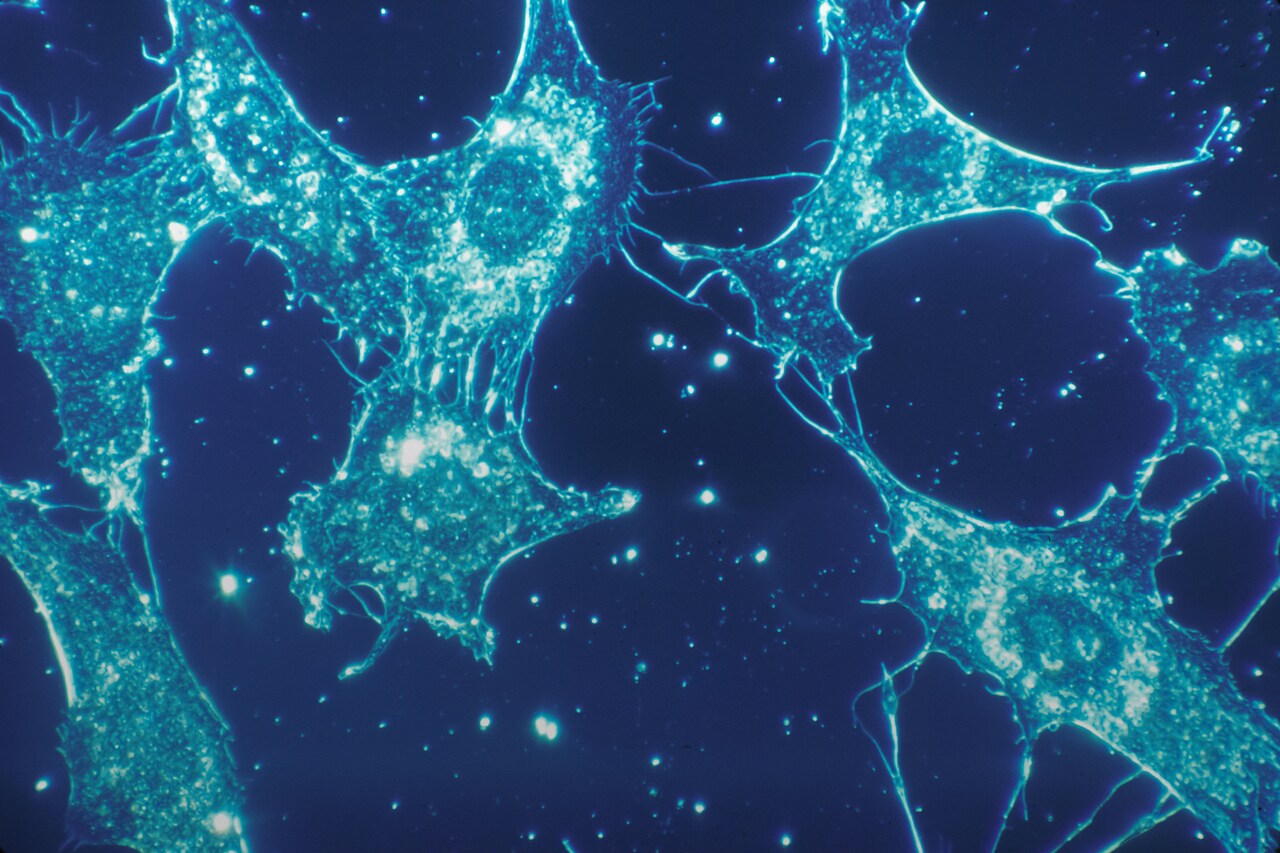
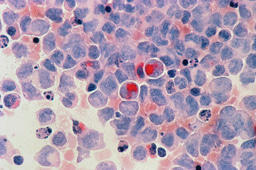
Socioeconomic status also divides cancer care in the same geographical region (Vaccarella et al., 2022). Innovative therapies like checkpoint inhibitors and CAR-T cell therapy are extremely expensive which further marginalises lower-income populations, who paradoxically often face greater disease burdens and worse prognoses (Ahmed et al., 2022). Pembrolizumab's inaccessible cost of $150,000 per patient annually in 2017, effectively excluded it as a treatment option in LMICs (Lai et al., 2023). Previously successful in Brazil (Nunn, Fonseca and Gruskin, 2009) and India (Kamiike, 2019), compulsory licensing as per the TRIPS Agreement, may resolve this dilemma. By enabling governments to manufacture generic copies of patented medicines during health crises, conventionally expensive cancer medications are made more accessible (Bognar, Bychkovsky and Lopes, 2016).
Equity in oncology is a global imperative, demanding urgent action. Employing resource-stratified models in oncology, decentralising clinical trials, and reforming drug pricing through compulsory licensing are pragmatic actions towards dismantling existing systemic inequalities. However, achieving this requires both evidence-based policy and political will, but also global collaboration (Edward Christopher Dee et al., 2023) that ensures future cancer care is shaped by need, not geography or wealth, addressing health inequities with fair and resource-driven solutions.
References:
Oluwaseun Adebayo Bamodu and Chung, C.-C. (2024). Cancer Care Disparities: Overcoming Barriers to Cancer Control in Low- and Middle-Income Countries. JCO Global Oncology, 10(10). doi:https://doi.org/10.1200/go.23.00439.
WHO (2018). Cancer. [online] WHO | Regional Office for Africa. Available at: https://www.afro.who.int/health-topics/cancer.
National Comprehensive Cancer Network (2025). Framework for Resource Stratification. [online] NCCN. Available at: https://www.nccn.org/global/what-we-do/nccn-framework-for-resource-stratification-of-nccn-guidelines?utm_source=chatgpt.com [Accessed 29 Feb. 2025].
De las Heras, B., Daehnke, A., Saini, K.S., Harris, M., Morrison, K., Aguilo, A., Chico, I., Vidal, L. and Marcus, R. (2022). Role of decentralized clinical trials in cancer drug development: Results from a survey of oncologists and patients. DIGITAL HEALTH, 8(8), p.205520762210999. doi:https://doi.org/10.1177/20552076221099997.
Duggan, C., Dvaladze, A., Rositch, A.F., Ginsburg, O., Yip, C., Horton, S., Camacho Rodriguez, R., Eniu, A., Mutebi, M., Bourque, J., Masood, S., Unger‐Saldaña, K., Cabanes, A., Carlson, R.W., Gralow, J.R. and Anderson, B.O. (2020). The Breast Health Global Initiative 2018 Global Summit on Improving Breast Healthcare Through Resource‐Stratified Phased Implementation: Methods and overview. Cancer, 126(S10), pp.2339–2352. doi:https://doi.org/10.1002/cncr.32891.
Msyamboza, K.P., Phiri, T., Sichali, W., Kwenda, W. and Kachale, F. (2016). Cervical cancer screening uptake and challenges in Malawi from 2011 to 2015: retrospective cohort study. BMC Public Health, 16(1). doi:https://doi.org/10.1186/s12889-016-3530-y.
Kamaraju, S., Drope, J., Sankaranarayanan, R. and Shastri, S. (2020). Cancer Prevention in Low-Resource Countries: An Overview of the Opportunity. American Society of Clinical Oncology Educational Book, (40), pp.72–83. doi:https://doi.org/10.1200/edbk_280625.
Hunter, N., Dempsey, N., Tbaishat, F., Jahanzeb, M., Al-Sukhun, S. and Gralow, J.R. (2020). Resource-Stratified Guideline-Based Cancer Care Should Be a Priority: Historical Context and Examples of Success. American Society of Clinical Oncology Educational Book, 40(40), pp.217–226. doi:https://doi.org/10.1200/edbk_279693.
Drain, P.K., Parker, R.A., Robine, M. and Holmes, K.K. (2018). Global migration of clinical research during the era of trial registration. PLOS ONE, 13(2), p.e0192413. doi:https://doi.org/10.1371/journal.pone.0192413.
Adams, D.V., Long, S. and Fleury, M.E. (2022). Association of Remote Technology Use and Other Decentralization Tools With Patient Likelihood to Enroll in Cancer Clinical Trials. JAMA Network Open, 5(7), p.e2220053. doi:https://doi.org/10.1001/jamanetworkopen.2022.20053.
Salako, O., Fagbenro, G., Joseph, A., Enyi, A.F., Adegboyega, B.C. and Okunade, K.S. (2023). An ehealth intervention during radical radiotherapy: Patient-Reported Outcome Side effects (PROSE) study—An emerging approach from sub-Saharan Africa. Journal of Clinical Oncology, 41(16_suppl), pp.6628–6628. doi:https://doi.org/10.1200/jco.2023.41.16_suppl.6628.
Ndembi, N., Mekonen, T.T., Folayan, M.O., Dereje, N., Kruger, A., Fokam, J., Temfack, E., Raji, T., Nachega, J., Boum, Y., Crowell, T.A., Ngongo, A.N., Mboup, S., Ntoumi, F., Loots, G., Makanga, M., Sow, S., Karim, S.A. and Nkengasong, J. (2024). Strengthening and expanding capacities in clinical trials: advancing pandemic prevention, preparedness and response in Africa. Nature Communications, 15(1). doi:https://doi.org/10.1038/s41467-024-53126-3.
Vaccarella, S., Georges, D., Bray, F., Ginsburg, O., Charvat, H., Martikainen, P., Brønnum-Hansen, H., Deboosere, P., Bopp, M., Leinsalu, M., Artnik, B., Lorenzoni, V., Vries, E.D., Marmot, M., Vineis, P., Mackenbach, J. and Nusselder, W. (2022). Socioeconomic inequalities in cancer mortality between and within countries in Europe: A population-based study. The Lancet Regional Health – Europe, [online] 0(0). doi:https://doi.org/10.1016/j.lanepe.2022.100551.
Ahmed, N., Shahzad, M., Shippey, E., Bansal, R., Mushtaq, M.U., Mahmoudjafari, Z., Faisal, M.S., Hoffmann, M., Abdallah, A.-O., Divine, C., Hamadani, M., McGuirk, J. and Shune, L. (2022). Socioeconomic and Racial Disparity in Chimeric Antigen Receptor T Cell Therapy Access. Transplantation and Cellular Therapy, [online] 28(7). doi:https://doi.org/10.1016/j.jtct.2022.04.008.
Lai, Y., Bensimon, A.G., Gao, E., Bhattacharya, R., Xu, R., Jestinah Chevure, Imai, K. and Haas, N.B. (2023). Cost-Effectiveness Analysis of Pembrolizumab as an Adjuvant Treatment of Renal Cell Carcinoma Post-nephrectomy in the United States. Clinical genitourinary cancer, 21(5), pp.612.e1–612.e11. doi:https://doi.org/10.1016/j.clgc.2023.03.016.
Nunn, A., Fonseca, E.D. and Gruskin, S. (2009). Changing global essential medicines norms to improve access to AIDS treatment: Lessons from Brazil. Global Public Health, 4(2), pp.131–149. doi:https://doi.org/10.1080/17441690802684067.
Kamiike, A. (2019). The TRIPS Agreement and the Pharmaceutical Industry in India. Journal of Interdisciplinary Economics, [online] 32(1), p.026010791987557. doi:https://doi.org/10.1177/0260107919875573.
Bognar, C.L.F.B., Bychkovsky, B.L. and Lopes, G. de L. (2016). Compulsory Licenses for Cancer Drugs: Does Circumventing Patent Rights Improve Access to Oncology Medications? Journal of Global Oncology, [online] 2(5), pp.292–301. doi:https://doi.org/10.1200/jgo.2016.005363.
Edward Christopher Dee, Ann, M., Patricia, J., Duvern Ramiah, Hubbard, A., Dominique, F., Sullivan, R., Aggarwal, A., Booth, C., Legaspi, G.D., Nguyen, P.L., Pramesh, C.S. and Grover, S. (2023). Leveraging national and global political determinants of health to promote equity in cancer care. Journal of the National Cancer Institute, 115(10). doi:https://doi.org/10.1093/jnci/djad123.
Shan Sunny is a Third-year MBChB student at the University of Leeds School of Medicine, with a dedicated focus on oncology and global health equity in cancer care. As President of Polygeia Leeds, a student-led think tank, he combines academic rigour with leadership in research-driven policy development. His work centres on advancing molecular oncology treatments while exploring strategies to make these innovations accessible across diverse healthcare settings. Shan’s research, conducted as an EXSEL Scholarship recipient, examines resource-stratification frameworks for clinical implementation and decentralised clinical trials to enhance both the development and delivery of cancer therapeutics. With a keen interest in innovative drug-development pathways and equitable access models, he is committed to research that bridges cutting-edge science with real-world patient benefit, regardless of geographical or socioeconomic constraints.

Join the FEBS Network today
Joining the FEBS Network’s molecular life sciences community enables you to access special content on the site, present your profile, 'follow' contributors, 'comment' on and 'like' content, post your own content, and set up a tailored email digest for updates.