Ensuring dignity in terminal cancer: the global palliative care equity fund
As part of World Cancer Day (4th Feb), the journal of Molecular Oncology invited researchers to take part in a writing competition aimed at highlight existing or future policies directed at making cancer treatment equally accessible to all patients both locally and globally. This entry, by Marco Cordani (Complutense University of Madrid, Spain), received the first prize.
Inequity in cancer care manifests starkly in its end stages. While high-income countries offer robust palliative support—integrating analgesia, antiemetics, and psychosocial interventions—low- and middle-income countries (LMICs) face a profound gap. The World Health Organization estimates that 80% of terminal cancer patients in LMICs lack access to oral morphine, a cornerstone of pain management costing mere cents per dose. This disparity, driven by regulatory barriers and supply chain failures, condemns millions to unrelieved suffering. To address this, I propose the Global Palliative Care Equity Fund (GPCEF), a policy to equitably deliver palliative care resources and training worldwide.
The GPCEF would establish a multilateral framework, funded by governments, industry, and global health entities, to procure and distribute essential palliative medications—morphine, ondansetron, lorazepam—to underserved regions. It would leverage existing infrastructure, training community health workers via a digital platform to administer these drugs safely, guided by evidence-based protocols (e.g., WHO’s analgesic ladder). For instance, a health worker in rural Malawi could titrate morphine for a metastatic breast cancer patient, supported remotely by a palliative specialist. This stratified approach targets the 7 million cancer patients requiring end-of-life care annually, prioritizing scalability and sustainability.
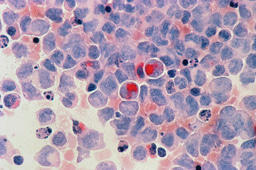
The policy’s future significance is rooted in epidemiology: cancer incidence in LMICs is projected to double by 2040, per GLOBOCAN data, amplifying palliative needs. GPCEF addresses this proactively, translating research—such as optimized opioid dosing or non-opioid adjuvants—into clinical practice. Unlike resource-intensive oncology units, it requires minimal capital; morphine’s production cost is trivial, yet its global availability remains curtailed by outdated narcotic policies. By reforming these regulations and establishing secure supply chains, GPCEF ensures access without risking diversion.
Implementation hurdles include opioid stigma, fragile health systems, and potential misuse. However, precedents like Uganda’s Hospice Africa model—integrating morphine into primary care—demonstrate feasibility. Mobile technology can mitigate connectivity issues, while blockchain-based tracking ensures transparency. Initial deployment in high-burden regions (e.g., South Asia) could validate efficacy, refining the model for global expansion.
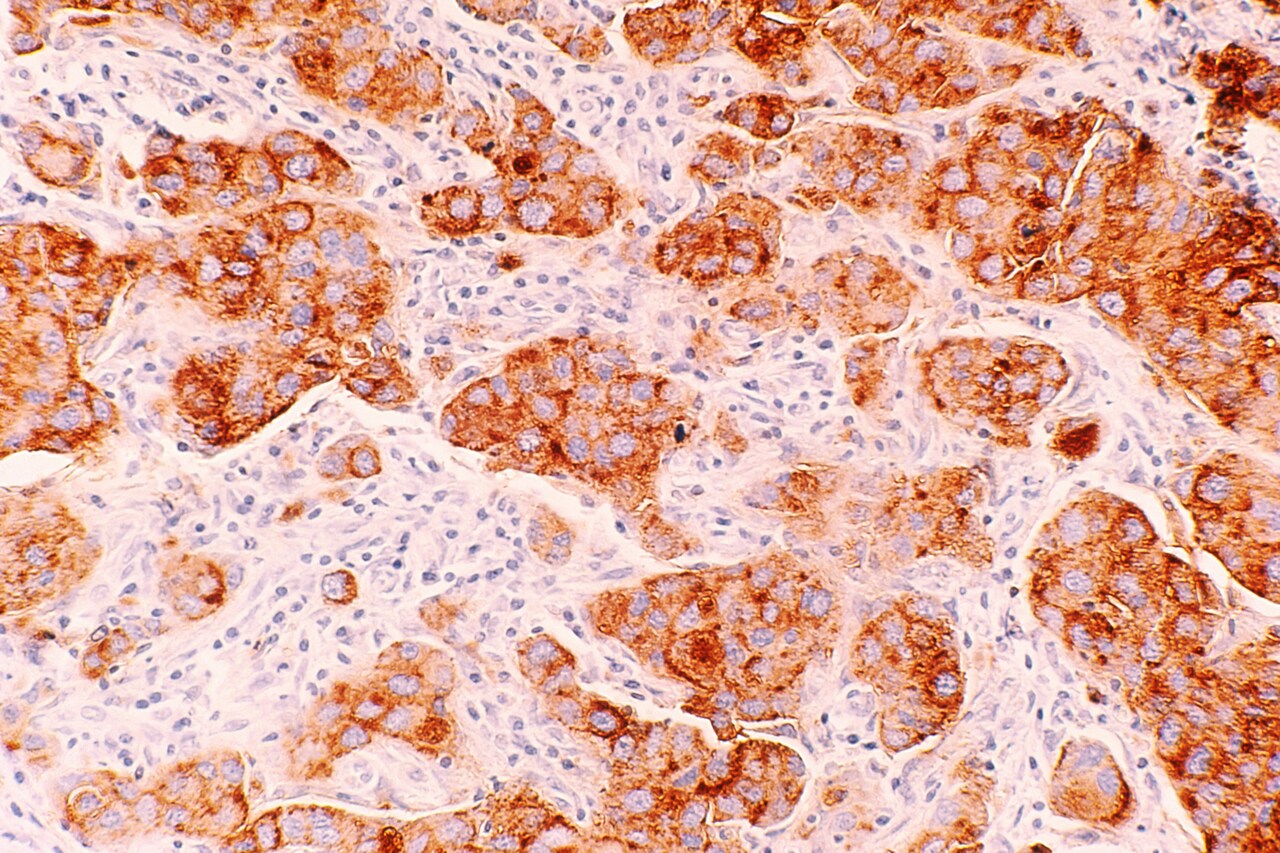
The scientific and humanitarian impact is transformative. Effective palliation reduces nociceptive and neuropathic symptom burdens, enhancing quality of life metrics (e.g., EORTC QLQ-C30 scores). It also generates real-world data on late-stage cancer phenotypes across diverse populations, potentially informing molecular research. Above all, GPCEF upholds equity by ensuring that socioeconomic status does not dictate dignity in death. In a field advancing targeted therapies, we must not neglect this fundamental duty: to alleviate suffering when curing is beyond reach.
Marco Cordani is a “Ramón y Cajal” researcher at the Complutense University of Madrid, Spain, where he teaches biochemistry and leads research on targeting cancer chemoresistance through autophagy modulation and the development of advanced drug delivery systems, including cannabinoid-loaded nanoparticles. He holds a PhD from the University of Verona, Italy, and has conducted postdoctoral research in Spain and France. His work has resulted in over 70 peer-reviewed publications in cancer research and pharmacology, and he maintains numerous international collaborations. He also serves as Associate Editor for Cell Communication and Signaling and Cancer Letters.
Join the FEBS Network today
Joining the FEBS Network’s molecular life sciences community enables you to access special content on the site, present your profile, 'follow' contributors, 'comment' on and 'like' content, post your own content, and set up a tailored email digest for updates.