How can self-driving car technology help personalized cancer medicine?

As part of World Cancer Day (4th Feb), the journal of Molecular Oncology invited researchers to take part in a writing competition aimed at highlighting how research in other areas of life sciences or technology influences the field of cancer biology and promotes cancer research. This entry, by Abraham Lin, received the first prize.
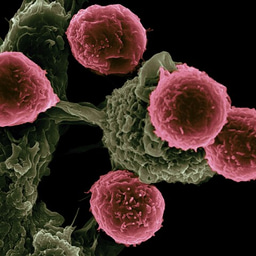
In the past, cancer medicine has generally been a “one-size-fits-all” approach, where a patient comes into the hospital and the doctor can only choose from a limited number of approved drugs or therapeutic strategies. Today, much more emphasis is being placed on personalized medicine, where doctors try to predict which strategy or drug will work the best for that individual patient. One method that holds great promise is through the use of “patient-derived organoids”, which are pieces of the patient tumor that can be grown in the lab to represent mini-patient tumors. Now, instead of having one chance to provide the patient with a successful drug, hundreds of drugs and drug combinations can be screened on these mini-patient tumors, and the best treatment strategy can be recommended to the doctor for that patient, based on how their organoids responded.
This is the goal of our research between Orbits and the Tumoroid Screening (TuSc) Lab at the University of Antwerp in Belgium. Despite the great potential and promise of patient-derived organoids for personalized medicine, one of the biggest barriers in their use is the lack of proper analysis to extract the valuable information they offer. The current method, called CellTiterGlo, destroys the organoids in the analysis process, flattens all the complexity of organoids into one readout, and can only be performed at one time-point. Altogether, these represent serious limitations and require you to choose a narrow window of observation. So how can we get more data out of the organoids?
By using computer vision and artificial intelligence, technology that is maturing in the self-driving car industry, Orbits has developed a method to analyze organoids without destroying them. Just as self-driving cars have “learned” to identify and classify various objects on the road (e.g. pedestrians, lane dividers, other cars), Orbits has developed an analysis method to learn to identify and classify various types of organoids in the lab, based on their specific features and structures. From microscope images of organoids taken continuously over time, Orbits can extract multiple data parameters about the organoids from the images, thus allowing for the monitoring and tracking of their growth without disruption. This has profound impacts in cancer drug screening and drug development, as it allows researchers to visualize how their drugs are affecting different patient organoids. We have already published that this method provides insight into the mechanisms of how different drugs work and whether there are drug-resistant regions within the patient tumor, all of which are significant advantages over the current organoid analysis methods. Our analysis methods can integrate into different microscope systems and works in a high-throughput manner, thereby allowing broad use for researchers, without having to buy additional (often expensive) microscope systems.
But how well does the behavior of patient-derived organoids in the lab, predict the behavior of patient tumors in the clinic? This is an ongoing research question at Orbits, TuSc Lab, and the University Hospital of Antwerp (UZA). While the Orbits organoid analysis can acquire multiple parameters from a drug screening experiment, we are now figuring out which parameters or combination of parameters have the most translatability to the patient that these organoids were derived from. In a small trial with 8 pancreatic cancer patients, we created organoids from their tumors and treated the organoids with the same therapies that the patients received in the clinic. We saw that by combining several organoid output parameters, our results in the lab had very high correlation with how all the patients responded to the therapies they received. We are now planning to set up larger clinical trials in which we can validate the predicative ability of our organoid image analysis outputs with patient response, as a big step towards more personalized medicine.
In the future, just as computer vision and artificial intelligence is revolutionizing the automotive industry, we believe these technologies will also make personalized cancer medicine a reality. We envision that one day, a cancer patient can walk into a clinic, a piece of their tumor will be taken to make organoids, and hundreds of drugs and drug combinations will be screened on their organoids. Based on how well their organoids respond to different treatment strategies in the lab, a recommendation will be made to their doctor for that specific patient. This would truly depart from the traditional “one-size-fits-all” approach of cancer treatment and move towards “individually-tailored” treatment strategies. For this to happen, much more collaboration and research with fields outside of cancer biology, such as computer vision, artificial intelligence, and biomedical engineering, is needed.
Photo by Samuele Errico Piccarini on Unsplash



Join the FEBS Network today
Joining the FEBS Network’s molecular life sciences community enables you to access special content on the site, present your profile, 'follow' contributors, 'comment' on and 'like' content, post your own content, and set up a tailored email digest for updates.